August 1, 2024
If you’ve been following Central Health news, you know that Travis County’s hospital district has opened 14 different specialty care and diagnostic lines of service. Five more are expected to go live by the end of September. At the beginning of 2023, we had none.
Central Health has soundly established itself as not just a planner and payor but also a provider of healthcare for Travis County’s residents with low income. But why so many specialties? Why bring them online so quickly? And why now?
Back in 2021-22, as part of the process that produced Central Health’s Healthcare Equity Plan, we conducted the first-ever Community Health Needs Assessment (CHNA, an established planning tool) specifically for Travis County’s safety-net healthcare population. That’s people living at 200% or less of the federal poverty level, which is roughly $30,000/year for an individual or $60,000/year for a family of four.

As you might anticipate, the medical needs of residents with low income are greater than those of Travis County at large. The safety-net population is younger, includes more childbearing women, and experiences a higher rate of many chronic conditions, including diabetes, hypertension, preventable cancers (breast, cervical, colorectal), and kidney disease. It also experiences a higher rate of behavioral health conditions and patients with substance use disorders. The life expectancy of this entire population is a decade less than the median for Travis County.
The Central Health system’s CommUnityCare Health Centers is the largest provider of preventive and primary care, including behavioral, dental, and women’s healthcare, for the safety-net population in Travis County. While the county still needs more primary care capacity, the gaps are smaller, the wait times are shorter for patients to be seen, and more people are served.
Specialty care is a different story. People with low income wait longer to seek medical care, which means their conditions become more advanced, and a specialist becomes more necessary. Podiatry, particularly for patients with uncontrolled diabetes, is a common case in point; lack of good care for the legs and feet leads to amputations that diminish the quality of life. Podiatry was the very first specialty care line Central Health established.
The CHNA bore out how vastly underserved safety-net patients were by Travis County’s specialty care providers. Across specialties from cardiology to gastroenterology to psychiatry to all kinds of surgery, Travis County needs dozens of physicians who take Medicaid or Central Health’s Medical Access Program (MAP) or MAP Basic coverage and focus on safety-net care. Currently, the county might have three, or one, or half of one who also practices elsewhere, or none.
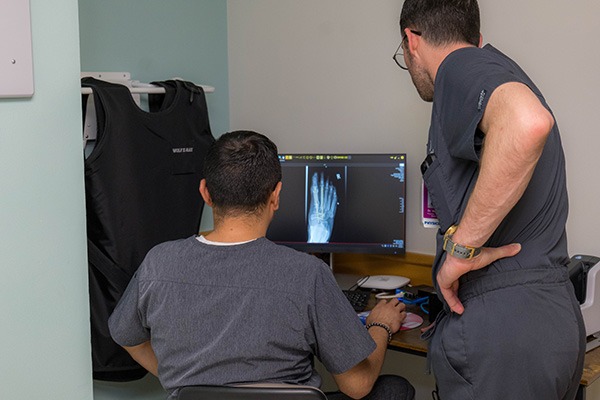
The total tally of needed specialty care physicians in the CHNA was 375. Central Health intends to hire those physicians as the district evolves into one of the most innovative and equity-focused specialty care practices in America. Each of those MDs or DOs needs a care team – physician’s assistants, advance practice nurses, RNs and LVNs, medical assistants, and social workers and community health workers. They’ll also need radiologists, X-ray technicians, pharmacists, testing lab techs, and more. It adds up to thousands of people that Travis County needs to deliver equitable care to its safety-net patients. Over the course of implementing the Healthcare Equity Plan (from now until 2030), Central Health will hire and employ most of those people as well.

Central Health had aimed to gradually staff up its specialty care practice, to make sure that these lines of service would be sustainable going forward 20 or 30 years from now. We had money that we would have spent on contracts for these specialty services if they were available, but they simply weren’t. We planned to use those reserves for the one-time costs of setting up lines of service, gradually calibrating them so that our property tax revenue could cover their ongoing costs.
This year, however, we decided to take a different tack, with the guidance and support of our previous President & CEO Mike Geeslin and our current leader Dr. Pat Lee. Ironically, the cash we’d set aside has grown along with hikes in interest rates, and Central Health’s medical leadership encouraged moving ahead to address the critical needs patients had now.
And so, as Central Health has opened one specialty line of care after another, patients who had been waiting a year or more for an appointment could now get one in two months, or two weeks, or even today, to get the care they have needed for so long. Every day that this care has been available has led to improved quality of life and hope of lengthened lifespans for the people we serve. It is only fair and equitable, and even ethical, to move with speed to get this done.
In August, Central Health’s first permanent multispecialty clinic will see its first patients at the former Rosewood-Zaragosa health center in East Austin. This new clinic represents a significant step forward in our mission to provide equitable healthcare for Travis County residents. Expected to handle between 25,000-40,000 visits annually, the clinic will dramatically reduce wait times for our MAP and MAP Basic members, in line with our Healthcare Equity Plan.